

Necessary cookies are absolutely essential for the website to function properly. *Commonly occurs in the metaphyseal region if there has been severe comminution, these injuries may require revision fixation and bone grafting ComplicationsĬommon complications following surgical repair include compartment syndrome, wound infection or dehiscence, delayed or non-union*, and post-traumatic arthritis. in older patients or where definitive fixation has failed), fusion of the ankle with a hindfoot nail may be warranted. When definitive fixation does take place, it is best performed under traction, such as that provided by an external fixator. Figure 2 – Plain film radiograph showing a right pilon fracture Management This involves the application of a temporary spanning external fixator followed by definitive fixation (ORIF) 7-14 days later once the soft tissues have had the opportunity to heal. Surgery aims to reconstruct the articular surface, restore the alignment of the ankle mortise, and protect the soft tissues around the ankle joint.Ī staged approach is often the preferred management option, especially if significant soft tissue swelling. The vast majority of pilon fractures are treated operatively, the timing of which depends on the degree of soft tissue involvement and the presence of any emergency complications (such as neurovascular injury). However, as these injuries are intrinsically unstable, loss of reduction and subsequent malunion is common. Simple undisplaced pilon fractures are rare but may be treated non-operatively, particularly in elderly patients and patients to whom an operation is very high risk. The limb must be elevated and monitored for compartment syndrome, and the patient kept nil by mouth with IV fluids in preparation for surgery. After which, a r epeat neurovascular assessment and check plain film radiographs should be performed.
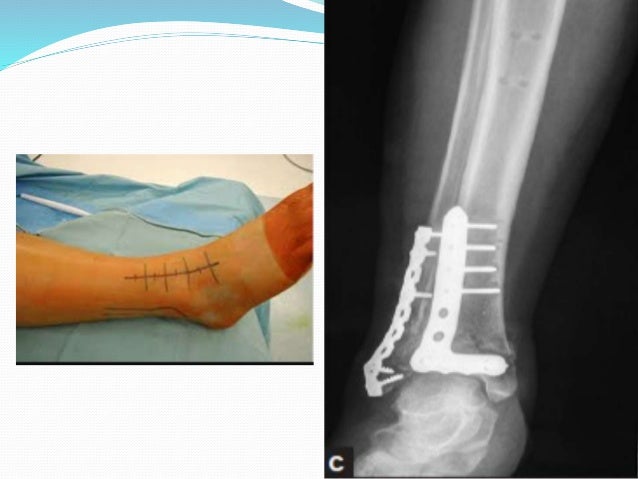
Intramedullary nail fixation: This involves insertion of a metal rod called an intramedullary nail into the hollow core of the bone that runs its length in order to provide stability while the fracture heals.External fixation: This technique involves affixing pins or screws externally to the bone, connected by an external frame, to provide protection and stability while the bone heals.Internal fixation: This involves stabilizing the bone with plates and screws placed internally to aid in healing.Physical therapy interventions may include a range of motion exercises, joint mobility exercises, flexibility and balance exercises, etc.
#Pilon fracture recovery blog full
Physical therapy: Physical therapy for a pilon fracture is essential to help the patient recover and regain full range of motion, strength, balance and function.This involves the doctor positioning the bone back into its normal alignment, followed by the application of a plaster cast to keep the bone in place while it heals. Closed reduction and Plaster casting: The most common treatment for a Pilon fracture is closed reduction and plaster casting.By using bone scans, doctors can evaluate the severity or presence of a bone fracture along with other associated conditions that may be present, such as infection or tumor. Bone scans: Bone scans are a type of imaging test that use a type of x-ray technology to produce detailed images of bones and the surrounding soft tissues.By assessing the displacement and orientation of the fracture fragments, the severity of the injury is determined. Fractured bones may often be visualized on CT scans due to their varying densities. CT scans: CT scans allow for detailed evaluation of the bone structure, including alignment.

MRI scans allow for detailed images of the bones to be obtained, so that the size and location of the fracture can be accurately determined. Magnetic resonance imaging ( MRI): MRI is very useful for detecting a Pilon fracture.X-rays: X-rays are typically used to diagnose a Pilon fracture, as they can reveal any fractures, displacement of the bones, and tell-tale signs of fractures such as bony debris around the fractured area.


 0 kommentar(er)
0 kommentar(er)
